Post #24 – My next Surgery
Dear Family and Friends
I kind of got off track these past few posts, so today I am
swinging back around a bit😊 so far
we have been over my diagnosis, my surgery for my post, the red devil
chemotherapy treatments, chemo brain, how laughter helps, how a great support
system helps (emotionally, mentally, spiritually, and physically), and today I
want to talk about my next surgery – these have all been a part of my cancer treatment.
"Another cosmic fact: only by aligning our wills with God’s is full happiness to be found. Anything less results in a lesser portion (see Alma 12:10–11). The Lord will work with us even if, at first, we “can no more than desire” but are willing to “give place for a portion of [His] words” (Alma 32:27). A small foothold is all He needs! But we must desire and provide it."

I don’t know if I mentioned to you that I would have to have my breast
removed because of the cancer. I was OK with that, I told the doctor that
he could take anything that he needed--that I didn’t need-- as long as it would
leave me more time with my family. So, now I will need to make another
appointment with my original surgeon. They were very kind from the office staff
to the nurses, and the doctor.
My daughter was there with me during this time as well.
Originally, they thought they would have to take both breasts, but decided
after the genetic tests that is was only necessary for them to take the one
that was cancerous. It had spread to my lymph nodes, so they couldn't
do just do a lumpectomy. for those of you who have not experienced or
known someone who has experienced a mastectomy -- here is some information for
you.
Overview
Mastectomy
A mastectomy is
surgery to remove all breast tissue from a breast as a way to treat or prevent
breast cancer.
For those with
early-stage breast cancer, a mastectomy may be one treatment option.
Breast-conserving surgery (lumpectomy), in which only the tumor is removed from
the breast, may be another option.
Deciding between a
mastectomy and lumpectomy can be difficult. Both procedures are equally
effective for preventing a recurrence of breast cancer. But a lumpectomy isn't
an option for everyone with breast cancer, and others prefer to undergo a
mastectomy.
Newer mastectomy
techniques can preserve breast skin and allow for a more natural breast
appearance following the procedure. This is also known as skin-sparing
mastectomy.
Surgery to restore
shape to your breast — called breast reconstruction — may be done at the same
time as your mastectomy or during a second operation at a later date.
"Another cosmic fact: only by aligning our wills with God’s is full happiness to be found. Anything less results in a lesser portion (see Alma 12:10–11). The Lord will work with us even if, at first, we “can no more than desire” but are willing to “give place for a portion of [His] words” (Alma 32:27). A small foothold is all He needs! But we must desire and provide it."
—Neal A. Maxwell, "Swallowed Up in the Willl of the Father"

Why it's done
A mastectomy is used
to remove all breast tissue if you have breast cancer or are at very high risk
of developing it. You may have a mastectomy to remove one breast (unilateral
mastectomy) or both breasts (bilateral mastectomy).
Mastectomy
for breast cancer treatment
A mastectomy may be a
treatment option for many types of breast cancer, including:
·
Ductal
carcinoma in situ (DCIS), or noninvasive breast cancer
·
Stages
I and II (early-stage) breast cancer
·
Stage
III (locally advanced) breast cancer — after chemotherapy
·
Inflammatory
breast cancer — after chemotherapy This is the type of cancer that I have so therefore the
reason for my mastectomy. This type of cancer is very aggressive and grows more
rapidly than other types of breast cancer as I have been told.
·
Paget's
disease of the breast
·
Locally
recurrent breast cancer
Your doctor may
recommend a mastectomy instead of a lumpectomy plus radiation if:
·
You
have two or more tumors in separate areas of the breast.
·
You
have widespread or malignant-appearing calcium deposits (microcalcifications)
throughout the breast that have been determined to be cancer after a breast
biopsy.
·
You've
previously had radiation treatment to the breast region and the breast cancer
has recurred in the breast.
·
You're
pregnant and radiation creates an unacceptable risk to your unborn child.
·
You've
had a lumpectomy, but cancer is still present at the edges (margin) of the
operated area and there is concern about cancer extending to elsewhere in the
breast.
·
You
carry a gene mutation that gives you a high risk of developing a second cancer
in your breast.
·
You
have a large tumor relative to the overall size of your breast. You may not
have enough healthy tissue left after a lumpectomy to achieve an acceptable
cosmetic result. This
too, was the reason given for my mastectomy, my tumor was so aggressive and
fast growing.
·
You
have a connective tissue disease, such as scleroderma or lupus, and may not
tolerate the side effects of radiation to the skin.
"The most important thing you can do is to learn to talk to God. Talk to Him as you would talk to your father, for He is your Father, and He wants you to talk to Him. He wants you to cultivate ears to listen, when He gives you the impressions of the Spirit to tell you what to do. If you learn to give heed to the sudden ideas which come to your minds, you will find those things coming through in the very hour of your need. If you will cultivate an ear to hear these promptings, you will have learned to walk by the spirit of revelation."
—Harold B. Lee, "Chapter 6: To Hear the Voice of the Lord"

Mastectomy
to prevent breast cancer
You might also
consider a mastectomy if you don't have breast cancer but have a very high risk
of developing the disease.
A preventive
(prophylactic) or risk-reducing mastectomy involves removing both of your
breasts and significantly reduces your risk of developing breast cancer in the
future.
A prophylactic
mastectomy is reserved for those with a very high risk of breast cancer, which
is determined by a strong family history of breast cancer or the presence of
certain genetic mutations that increase the risk of breast cancer.
Risks
Risks of a mastectomy
include:
·
Bleeding
·
Infection
·
Pain
·
Swelling
(lymphedema) in your arm if you have an axillary node dissection
·
Formation
of hard scar tissue at the surgical site
·
Shoulder
pain and stiffness
·
Numbness,
particularly under your arm, from lymph node removal
·
Buildup
of blood in the surgical site (hematoma)
"Acknowledge and face your weaknesses, but don’t be immobilized by them, because some of them will be your companions until you depart this earth life. No matter what your current status, the very moment you voluntarily choose honest, joyful, daily repentance by striving to simply do and be your very best, the Savior’s Atonement envelops and follows you, as it were, wherever you go. Living in this manner, you can truly “always retain a remission of your sins” (Mosiah 4:12) every hour of every day, every second of every minute, and thus be fully clean and acceptable before God all the time."
—Jörg Klebingat, "Approaching the Throne of God wth Confidence"

How you prepare
Meet
with your surgeon to discuss your options
Before your surgery,
you'll meet with a surgeon and an anesthesiologist to discuss your operation,
review your medical history and determine the plan for your anesthesia.
This is a good time
to ask questions and to make sure you understand the procedure, including the
reasons for and risks of the surgery.
One issue to discuss
is whether you'll have breast reconstruction and when. One option may be to
have the reconstruction done immediately after your mastectomy, while you're
still anesthetized.
The first time I went in to see the surgeon about the breast removal, there were two women there to guide me through the process, which was very helpful for me. They gave me their cards, so I could call if I needed anything.
"You are never lost when you can see the temple. The temple will provide direction for you and your family in a world filled with chaos. It is an eternal guidepost which will help you from getting lost in the “mist of darkness.” It is the house of the Lord. It is a place where covenants are made and eternal ordinances are performed."
—Gary E. Stevenson, "Sacred Homes, Sacred Temples"

Breast reconstruction
may involve:
·
Using
breast expanders with saline or silicone implants As I understand it,
they could not do this for me because of the radiation that I would be
undergoing after my mastectomy.
·
Using
your body's own tissue (autologous tissue reconstruction) They could not save
any of my breast tissue because it was all cancerous. It is amazing the things
you learn after the fact😊
·
Using
a combination of tissue reconstruction and implants
Breast reconstruction
is a complex procedure performed by a plastic surgeon, also called a
reconstructive surgeon. If you're planning breast reconstruction at the same
time as a mastectomy, you'll meet with the plastic surgeon before the surgery.
Preparing
for your surgery
You'll be given
instructions about any restrictions before surgery and other things you need to
know, including:
·
Tell your doctor about any medications, vitamins or
supplements you're taking. Some substances could interfere with the surgery.
·
Stop taking aspirin or other blood-thinning medication. A week or
longer before your surgery, talk to your provider about which medications to
avoid because they can increase your risk of excessive bleeding. These include
aspirin, ibuprofen (Advil, Motrin IB, others) and other pain relievers, and
blood-thinning medications (anticoagulants), such as warfarin (Coumadin,
Jantoven).
·
Don't eat or drink 8 to 12 hours before surgery. You'll receive
specific instructions from your health care team.
·
Prepare for a hospital stay. Ask your doctor
how long to expect to stay in the hospital. Bring a robe and slippers to help
make you more comfortable in the hospital. Pack a bag with your toothbrush and
something to help you pass the time, such as a book.
"The Atonement is for you and for me. It is an enabling and a redeeming power. If you are not feeling worthy to stand in holy places, do not carry this burden one day longer. In mortality, we will all make mistakes. Be assured that the Savior loves you so much that He made it possible for you to change and to repent if you make a mistake. Satan does not want you to think you can change. He will try to convince you that all is lost. That is a lie. You can return. You can repent. You can be pure and holy because of the Savior’s infinite Atonement."
—Elaine S. Dalton, "Be Not Moved!"

What you can expect
 https://www.mayoclinic.org/tests-procedures/mastectomy/about/pac-20394670
https://www.mayoclinic.org/tests-procedures/mastectomy/about/pac-20394670
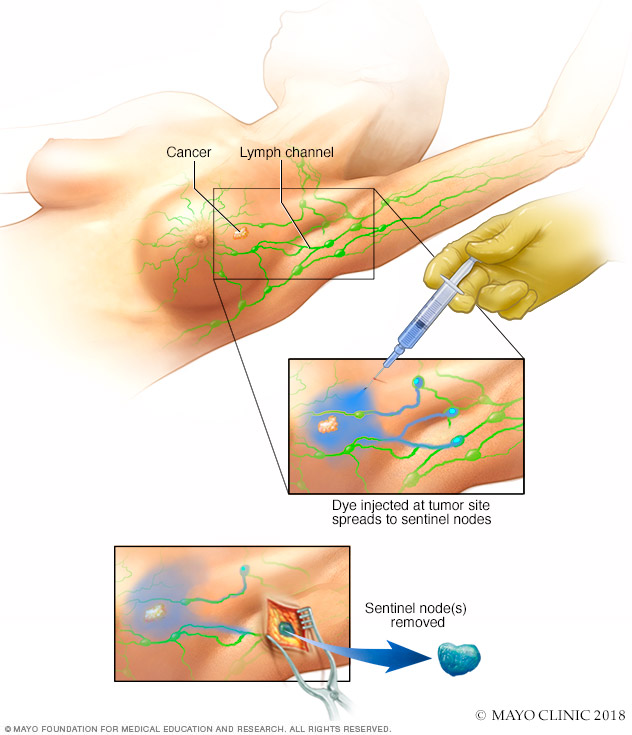
Sentinel node biopsy
A mastectomy is an
umbrella term used for several techniques to remove one or both breasts. In
addition, the surgeon may also remove nearby lymph nodes to determine whether
the cancer has spread.
During an axillary
node dissection, the surgeon removes a number of lymph nodes from your armpit
on the side of the tumor.
In a sentinel lymph
node biopsy, your surgeon removes only the first few nodes into which a tumor
drains (sentinel nodes).
Lymph nodes removed
during a mastectomy are then tested for cancer. If no cancer is present, no
further lymph nodes need be removed. If cancer is present, the surgeon will
discuss options, such as radiation to your armpit. If this is what you decide
to do, no further lymph nodes will need to be removed.
Removing all of the
breast tissue and most of the lymph nodes is called a modified radical
mastectomy. Newer mastectomy techniques remove less tissue and fewer lymph
nodes. The
doctor told me during my recovery from surgery that they had to take all of my
lymph nodes because they were all cancerous. So, instead of having a simple radical mastectomy I ended up having a modified
radical mastectomy.
"It should be obvious to each of us that our ultimate friendship should be with our Heavenly Father and His Son, Jesus Christ. The Savior has affectionately said to us, “I will call you friends, for you are my friends” (D&C 93:45). His greatest desire for us, His brothers and sisters, is to bring us back to our Father. And the way for us is clear: develop in our lives, to the degree that we can, the qualities and attributes of Christ. Obey His commandments and do His work and His will."
Other types of mastectomy
include:
·
Total mastectomy. A total mastectomy, also known as
a simple mastectomy, involves removal of the entire breast, including the
breast tissue, areola and nipple. A sentinel lymph node biopsy may be done at
the time of a total mastectomy.
·
Skin-sparing mastectomy. A skin-sparing mastectomy
involves removal of all the breast tissue, nipple and areola, but not the
breast skin. A sentinel lymph node biopsy also may be done. Breast
reconstruction can be performed immediately after the mastectomy.
A skin-sparing mastectomy may not be
suitable for larger tumors.
·
Nipple-sparing mastectomy. A nipple- or areola-sparing
mastectomy involves removal of only breast tissue, sparing the skin, nipple and
areola. A sentinel lymph node biopsy also may be done. Breast reconstruction is
performed immediately afterward.

Before
the procedure
Your doctor or nurse
will tell you when to arrive at the hospital. A mastectomy without
reconstruction usually takes one to three hours. The surgery is often done as
an outpatient procedure, and most people go home on the same day of the
operation.
If you're having both
breasts removed (a double mastectomy), expect to spend more time in surgery and
possibly an additional day in the hospital. If you're having breast
reconstruction following a mastectomy, the procedure also takes longer and you
may stay in the hospital for a few additional days.
If you're having a
sentinel node biopsy, before your surgery a radioactive tracer and a blue dye
are injected into the area around the tumor or the skin above the tumor. The
tracer and the dye travel to the sentinel node or nodes, allowing your doctor
to see where they are and remove them during surgery.
So, my appointment was made, and I went in to the hospital on
December 19, 2015. They visited with me for a while, put in the IV and pretty
soon I was ready to be taken down to the surgical unit. I know that I was awake
for a short while, after I went to the surgical unit, but I’m not sure just for
how long. When the surgery was done, I awoke in the hospital room where I would stay for a few
days.

During
the procedure
A mastectomy is
usually performed under general anesthesia, so you're not aware during the
surgery. Your surgeon starts by making an elliptical incision around your
breast. The breast tissue is removed and, depending on your procedure, other
parts of the breast also may be removed.
Regardless of the
type of mastectomy you have, the breast tissue and lymph nodes that are removed
will be sent to a laboratory for analysis.
If you're having
breast reconstruction at the same time as a mastectomy, the plastic surgeon
will coordinate with the breast surgeon to be available at the time of surgery.
One option for breast
reconstruction involves placing temporary tissue expanders in the chest. These
temporary expanders will form the new breast mound.
For women who will
have radiation therapy after surgery, one option is to place temporary tissue
expanders in the chest to hold the breast skin in place. This allows you to
delay final breast reconstruction until after radiation therapy.
If you're planning to
have radiation therapy after surgery, meet with a radiation oncologist before
surgery to discuss benefits and risks, as well as how radiation will impact
your breast reconstruction options. I am sure that they did, but I do not
remember them to have ever talked with me about breast reconstruction prior to
the surgery. I asked my daughter and she said that they mentioned it briefly
and gave me pamphlet but that was all that was ever said about breast
reconstruction. See how important it is to have an extra set of eyes and ears
at your appointments.
As the surgery is
completed, the incision is closed with stitches (sutures), which either
dissolve or are removed later. You might also have one or two small plastic
tubes placed where your breast was removed. The tubes will drain any fluids
that accumulate after surgery. The tubes are sewn into place, and the ends are
attached to a small drainage bag. These bags are for you to empty each time
they fill up, but it wasn’t too bad for me. You just do what you got to do –
right?

After
the procedure
After your surgery,
you can expect to:
·
Be
taken to a recovery room where your blood pressure, pulse and breathing are
monitored
·
Have
a dressing (bandage) over the surgery site
·
Feel
some pain, numbness and a pinching sensation in your underarm area
·
Receive
instructions on how to care for yourself at home, including taking care of your
incision and drains, recognizing signs of infection, and understanding activity
restrictions
·
Talk
with your health care team about when to resume wearing a bra or wearing a
breast prosthesis
·
Be
given prescriptions for pain medication and possibly an antibiotic
When the doctor came in to visit with me I had tubes coming out of
my front where my breast used to be as well as one on the side under my arm where
my lymph nodes used to be. He said that they had to take all of my lymph node
on that side because they were all cancerous. they did tests on everything while I was under anesthesia. Did you know how they determine how much of the breast to take? I was told that they only take as much as is cancerous. I asked this question because of the odd little blob of tissue in my underarm area. I asked why the doctor left it there when he could have easily shaped it better -- so weird, right?
It was very painful recovery as it was extremely sore for two
weeks, so I had to be off work for two weeks until the doctor took the tubes
out after they stopped draining. for those of you who have not experienced or
known someone who has experienced a mastectomy -- here is some information for
you.
Results
The results of your
pathology report should be available within a week or two after your
mastectomy. At your follow-up visit, your doctor can explain the report.
If you need more
treatment, your doctor may refer you to:
·
A radiation oncologist to discuss radiation treatments,
which may be recommended if you had a large tumor, many lymph nodes that tested
positive for cancer, cancer that had spread into the skin or nipple, or cancer
remaining after the mastectomy
·
A medical oncologist to discuss other forms of
treatment after the operation, such as hormone therapy if your cancer is
sensitive to hormones or chemotherapy or both
·
A plastic surgeon, if
you're considering breast reconstruction
-- I have gone
to see a breast reconstruction specialist – plastic surgeon, but she told me
that I would have to wait a year after the radiation was completed before
breast reconstruction would be an option for me. My son went with e to this
appointment and even he thought that the reconstruction would be a very hard
process to undergo – with any of the options that she presented to
us. I know that this is different for every woman, hopefully I have
given you some information that is helpful to you in making your decisions.
·
A counselor or support group to help you
cope with having breast cancer
It seems as if cancer
is so much more prevalent now a day than it used to be, or maybe its just that
we are more aware of it now than when my mother had her cancer back in the 70’s,
I wonder? I see more movies with cancer patients in them as well as more commercials
about cancer – especially breast cancer.
Shoot just
since my diagnosis in 2015 I have 7 different people in my life who have been
diagnosed with different forms of cancer. These are people that I know well, most
are friends, and one is my sister – who was recently diagnosed with HER-2
positive breast cancer. Wow! So out of a
group of twenty people – seven have cancer. How many people do you know who
have some form of cancer? I will leave you today with this bit of information
on mastectomy and my thoughts on the frequency of cancer that seems to be going
on now, of course it might be just me. Make it a great week everybody😊




No comments:
Post a Comment